A history of Diabetes
The Ebers’ papyrus refers to a condition that resembles diabetes. The recommended treatment lasted for four days and included a liquid layer of bones, wheat, grass and earth.
Hindus write in the Ayur Veda that flies and ants are attracted to the sweet urine of people suffering from a mysterious disease.

The term diabetes (meaning “to pass through”) is used for the first time by the Greek physician Arateus of Capadocia to describe a condition of excessive urination.
The association of excessive urination and sweet urine is first described in Sanskrit literature by Indian physicists Susruta and Charuka. For the first time, urine is described as having the taste of honey.
Persian polymath Avicenna describes diabetes in great detail. He mentions two complications, gangrene and erectile dysfunction, and recommends treatment with a mixture of lupine and other seeds, which have a mild blood glucose lowering effect.

Swiss physician Paracelsus reports the presence of an abnormal substance in the urine of people with diabetes that remains as a residue after evaporation. He identifies the substance as a salt and attributes the development of diabetes to the deposition of this salt in the kidneys.
English Physician Thomas Willis notes several observations about diabetes that remain relevant today. His findings result in urine testing becoming mandatory in clinical examinations.

English physician and philosopher Matthew Dobson identifies a substance in the blood of people with diabetes that gives it a sweet taste. He proves that this substance is glucose and demonstrates for the first time that diabetes is a systemic disease and not one that originates in the kidneys.
English physican John Rollo treats people with diabetes with restrictive carbohydate diets and substances that moderate appetite. This improves the condition in some of his patients.

French physiologist Claude Bernard observes that sugar in urine is stored in the liver in the form of glycogen. This indicates that the central nervous system is involved in the regulation of blood glucose.

German physiologist Paul Langerhans first describes and isolates a cluster of cells in the pancreas that are subsequently found to secrete insulin. They are named after him as the Islets of Langerhans.
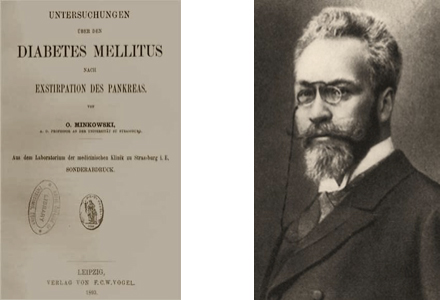
German physician Oscar Minkowski, along with Josef von Mering, is the first to establish the direct relationship between the pancreas and diabetes. They demonstrate this by removing the pancreas of a dog, which causes onset of diabetes.

1908 – German physican George Ludwig Zuelzer successfully produces a preparation from the pancreas that, when injected, prevents blood glucose levels from rising in people with diabetes. Unfortunately, he fails to establish the therapeutic value of his product due to side effects which follow its administration.
American physicians Frederick Allen and Elliott Joslin promote repeated fasting and prolonged undernutrition to treat diabetes. Although the evidence was poor that this was effective, it was viewed as the only possible treatment at the time.
Romanian physician Nicolae Paulescu discovers a hormone released by the pancreas that has a normalising effect on blood glucose levels. He names the hormone pancreine. In 1923, when Banting and Macleod are awarded the Nobel Prize for developing therapeutic insulin, Paulescu writes to the Nobel Prize committee claiming that he had discovered and used insulin first. His claims were rejected, but his achievements are subsequently recognised as significant in the history of diabetes.
Canadian surgeon Frederick Banting conceives the idea to ligate the pancreatic ducts of a dog and extract and isolate the secretions produced, for potential use as a treatment for diabetes.
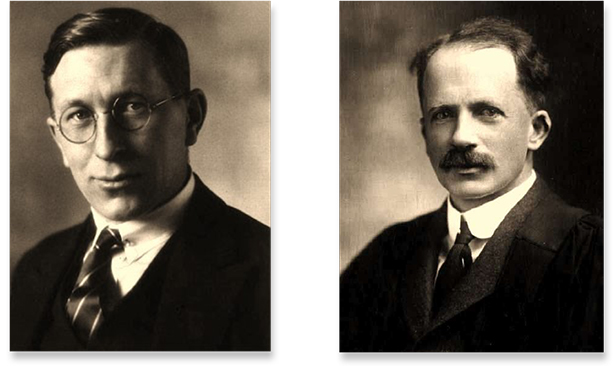
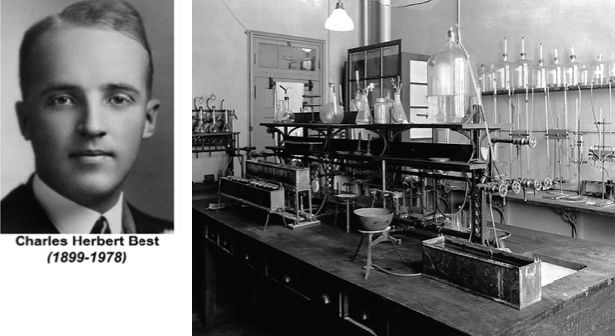
Banting conducts his experiments, assisted by Charles Best and supported by John JR Macleod. James Collip subsequently joins the research team to purify the pancreatic extract for clinical testing in humans.
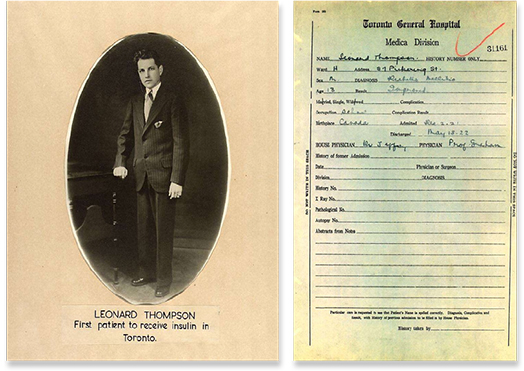
14-year old Leonard Thompson is successfully administered an injection of the pancreatic extract developed by Banting, Best and Collip. The extract is subsequently called insulin.
Danish pharmacologist Hans Hagedorn and colleagues discover that the effects of injected insulin can be prolonged by adding protamine to insulin. This extended duration insulin is called “Neutral Protamine Hagedorn” (NPH) insulin.
Tablets for testing glucose levels in urine become widely available. Urine test strips are subsequently developed in the 1950s.
The first standardized insulin syringe is produced. This reduces dosing errors and the associated episodes of high and low blood glucose.
Dr. Rachmiel Levine discovers that insulin works “like a key,” opening the door to transport glucose into the body’s cells. His research lays the groundwork for subsequent discoveries of the complex process involved in glucose transport.
The first oral medications – sulfonylureas – for type 2 diabetes become available. These stimulate the pancreas to release more insulin.
Drs Solomon Berson and Rosalyn Yalow develop a method for measuring insulin in the blood using radioimmunoassay technology. They notice that some people with diabetes continue to produce their own insulin and identify “insulin-dependent” (type 1) and “non-insulin-dependent” (type 2) diabetes.
Glucagon, a hormone produced by the pancreas that raises glucose levels, is introduced as a treatment for severe low blood glucose (hypoglycemia).
The first strips for testing blood glucose are introduced. These are initially used only in hospitals and clinics and subsequently become available for home use in the 1970s.
The first blood glucose meter is introduced for use in a clinical environment. Home glucose meters are subsequently made available in 1981, allowing people with diabetes to check their blood glucose levels more accurately and frequently.

A new concentration of insulin – U100 – is introduced. Insulin had previously been widely used in two different concentrations, U40 and U80, which required different syringes. The availability of this new single concentration, and insulin syringes marked with only a U100 scale, significantly reduces the frequency of dosing errors.
Continuous glucose monitoring and insulin infusion are made available, helping to significantly advance research into the nature of diabetes.
The first wearable medical infusion pumps are developed. These are capable of delivering biological materials such as chemotherapy drugs and insulin.
The glycosylated hemoglobin (HbA1C) test is developed. It subsequently becomes the standard test to measure long-term diabetes control.
Portable insulin pumps are introduced, allowing people with diabetes that use them to achieve normal blood glucose levels. They are, however, impractical due to their large size.

Researchers in California, USA, induce E. coli bacteria to produce insulin identical to human insulin. This is known as synthetic insulin.
Intensive insulin therapy, using the basal-bolus concept, is introduced as an effective treatment for people with type 1 diabetes
Human insulin produced by genetically altered bacteria is approved for therapeutic use. This largely eliminates adverse reactions caused by animal insulins.
The first insulin pen is introduced. It features a dial-up setting to measure the required dose and offers more accurate and convenient insulin delivery.

The incretin hormone GLP-1 is discovered. Incretin hormones encourage the body to produce insulin in response to food. This discovery leads to the subsequent development of a new class of oral medicines for type 2 diabetes that can increase insulin secretion in response to glucose.
The Diabetes Control and Complications Trial (DCCT) shows that keeping blood glucose levels as close to normal as possible slows the onset and progression of diabetes complications in people with type 1 diabetes.
Metformin, a biguanide that prevents glucose production in the liver, becomes the second type of oral medication approved to treat type 2 diabetes.
Lispro, a fast-acting insulin, is introduced.
The United Kingdom Prospective Diabetes Study (UKPDS) shows that people with type 2 diabetes who keep tight control of their blood glucose and blood pressure levels have a reduced risk of complications.
Lantus is introduced as the first analog basal, long-acting insulin.
The first in a new class of oral medications, DPP-4 inhibitors, is approved for therapeutic use in people with type 2 diabetes. These inhibitors enhance the body’s ability to lower elevated blood glucose levels.
The first in a new class of oral medications, SGLT-2 inhibitors, is approved for therapeutic use in people with type 2 diabetes. These inhibitors help lower elevated blood glucose levels by blocking the activity of sodium glucose transport proteins in the kidney.
Acknowledgements and sources:
- Prof. Luiz Gardete Correia, President Ernesto Roma Foundation
- https://www.diabetes.org/resources/timeline
The Insulin at 100 campaign is supported by



